The peripheral nervous system encompasses nerves outside the brain and spinal cord. It includes cranial nerves and spinal nerves. Motor neuron dysfunction leads to muscle weakness or paralysis, while sensory neuron dysfunction results in abnormal or lost sensation. Disorders can be generalized, symmetrical, or focal/multifocal.
Neuralgia
Neuralgia refers to stabbing, burning pain along a damaged nerve.
Clinical Presentation: Sudden, severe pain in specific nerve distributions (e.g., trigeminal nerve and intercostal neuralgia). Neuropathic pain within the area of sensory loss. Deep pain in the affected extremity.
Diseases with Neuralgia:
- Trigeminal neuralgia is associated with pain from the trigeminal nerve, often due to a blood vessel pressing on the nerve near the brainstem.
- Intercostal neuralgia is nerve pain that affects the area below the ribs and can be caused by several different conditions. In the context of a herpetic infection, it can manifest as a type of intercostal neuralgia known as postherpetic neuralgia. This condition arises after a shingles (herpes zoster) infection, leading to neuropathic pain along the intercostal nerves. Patients may experience sharp, stabbing, aching, or burning pain in the chest, upper trunk, or abdomen. Other symptoms may include itchiness, numbness, and restricted mobility of the shoulders and back.
Mononeuritis
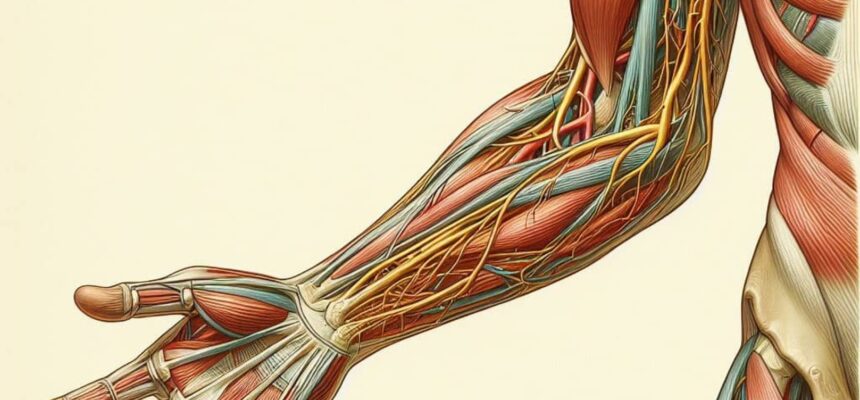
Mononeuritis is a term that describes a group of peripheral nerve disorders that cause sensory and motor deficits in the distribution of specific nerves. It can be caused by various conditions, such as vasculitis, diabetes, infections, or drugs. Mononeuritis can be classified into two types: mononeuritis simplex and mononeuritis multiplex. Mononeuritis simplex affects only one nerve, while mononeuritis multiplex affects two or more nerves in different areas of the body.
The symptoms of mononeuritis depend on the type and location of the affected nerves. They may include numbness, weakness, pain, tingling, or discomfort in the involved areas. The most frequently affected nerves are the median, ulnar, radial, peroneal, and sciatic nerves. Cranial nerves may also be involved, causing facial paralysis, hearing loss, or visual disturbances.
The workout for mononeuritis involves a detailed history and physical examination, as well as electrophysiological and laboratory tests. The history should elicit any risk factors or predisposing conditions for mononeuritis, such as diabetes, rheumatoid arthritis, lupus, or exposure to drugs or toxins. The physical examination should assess the sensory and motor functions of the affected nerves, as well as the reflexes and the vascular status of the limbs. The electrophysiological tests, such as nerve conduction studies (electromyography), can confirm the diagnosis of mononeuritis and determine the extent and severity of the nerve damage. The laboratory tests, such as blood chemistry, sedimentation rate, rheumatoid factor, thyroid function, and antinuclear antibodies, can help identify the underlying cause of mononeuritis and rule out other differential diagnoses.
The differential diagnosis of mononeuritis includes other peripheral neuropathies, such as polyneuropathy, radiculopathy, plexopathy, or entrapment neuropathy. These conditions can be distinguished from mononeuritis by their clinical presentation, electrophysiological findings, and response to treatment. For example, polyneuropathy usually affects both sensory and motor fibers in a symmetrical and distal pattern, while mononeuritis affects only certain nerves in an asymmetrical pattern. Radiculopathy affects the nerve roots at the spinal level, while mononeuritis affects the peripheral nerves at the limb level. Plexopathy affects the nerve plexuses, such as the brachial or lumbosacral plexus, while mononeuritis affects the individual nerves that branch from the plexus. Entrapment neuropathy affects the nerves at specific sites of compression, such as the carpal tunnel or the cubital tunnel, while mononeuritis affects the nerves at random locations.
The treatment of mononeuritis depends on the underlying cause and the severity of the symptoms. The main goals of the treatment are to control the inflammation, prevent further nerve damage, relieve the pain, and improve the function of the affected nerves. The treatment may include anti-inflammatory drugs, such as corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), or immunosuppressive agents, used to reduce the inflammation and swelling of the nerves. Analgesics, such as acetaminophen (paracetamol), ibuprofen, or opioids, may be used to relieve the pain and discomfort. Anticonvulsants, such as gabapentin, pregabalin, or carbamazepine, or antidepressants, such as amitriptyline, duloxetine, or venlafaxine, may be used to treat the neuropathic pain. Antiviral or antibacterial drugs may be used to treat the infections that cause mononeuritis. Physical therapy may be helpful to improve the strength, range of motion, and coordination of the affected muscles and joints. Physical therapy may also include exercises, massage, heat, cold, electrical stimulation, or ultrasound to enhance the blood circulation and nerve regeneration. Physical therapy may also provide education and advice on how to prevent further nerve injury, such as avoiding pressure, trauma, or repetitive movements of the affected areas. Surgery may be indicated for some cases of mononeuritis, especially when the nerve damage is severe or irreversible. Surgery may involve decompression, repair, or grafting of the damaged nerves. Surgery may also involve removal of tumors, cysts, or other masses that compress or infiltrate the nerves. Surgery may also involve amputation of the affected limbs, if they are severely infected, necrotic, or gangrenous. Surgery may improve the pain and function of the affected nerves, but it may also cause complications, such as infection, bleeding, or nerve injury. Therefore, surgery is usually considered as a last resort, when other treatments have failed or are contraindicated.
Plexitis
Brachial plexitis refers to sudden inflammation or injury to the brachial plexus—a network of nerves that control movement and sensation in the arm and hand. It often occurs due to trauma, viral infections (such as herpes zoster), or autoimmune processes.
Symptoms:
- Severe Pain: Intense pain in the upper arm or shoulder.
- Weakness: Muscle weakness or paralysis in the affected arm.
- Loss of Sensation: Diminished feeling in the arm.
Workout and Treatment:
- Physical Therapy: Helps maintain joint mobility and muscle strength.
- Immobilization: Resting the affected limb during the painful phase.
- Analgesics: Pain relief during the acute phase.
- Nerve Repair: Surgical reattachment of torn nerve ends.
- Nerve Graft: Using healthy nerves from elsewhere to bridge the gap.
- Tendon and Muscle Transfer: Transferring healthy tendons or muscles to restore function.
Mild cases may heal without intervention, while severe cases require specialized care.
Verified by Dr. Petya Stefanova