Status epilepticus (SE) presents a critical neurological condition characterized by prolonged or recurrent seizures without sufficient time for recovery between episodes. While more commonly observed in individuals with epilepsy, various factors can trigger continuous or repeated seizures in those without a prior history of epilepsy, rendering SE a life-threatening medical emergency requiring immediate intervention.
The definition of SE has evolved over time, with the focus primarily on the duration of seizure activity. Traditionally, SE was characterized by prolonged or recurrent seizures leading to an enduring epileptic state. If a seizure persists for more than five minutes or if back-to-back seizures occur without full consciousness restoration, prompt medical attention, typically through emergency services, is imperative.
Although relatively uncommon, SE constitutes one of the most prevalent brain-related emergencies, estimated that around 2% of seizures escalate into SE, and approximately 23% of new seizure cases involve this severe condition. SE is associated with considerable morbidity and mortality, necessitating timely recognition and intervention.
Causes and risk factors
Status epilepticus (SE) can arise from various underlying causes, particularly seizures, which are the primary trigger for this condition. Seizures can occur in two main ways, leading to the onset of SE: provoked seizures and unprovoked seizures.
Provoked seizures stem from other medical conditions or circumstances, such as high fevers, alcohol or drug withdrawal, low blood sugar levels, strokes, tumors, or encephalitis. Notably, when a brain injury provokes a seizure, it’s categorized as an acute symptomatic seizure, carrying a heightened risk of progressing to status epilepticus.
On the other hand, unprovoked seizures occur spontaneously, independent of any current medical conditions or circumstances. These seizures are indicative of an inherent susceptibility to seizure activity within the brain.
Children primarily experience status epilepticus due to fever-related infections, with severe, refractory seizure disorders also contributing to its occurrence.
Numerous risk factors heighten the susceptibility to status epilepticus. These encompass
-
poorly controlled epilepsy
- withdrawal from antiseizure medications
-
low blood sugar levels
-
stroke
-
kidney or liver failure
-
encephalitis
-
HIV infection
-
substance abuse
-
head injuries
Symptoms
The symptoms of status epilepticus encompass a range of manifestations, including
-
muscle spasms
-
falling
-
confusion
-
unusual noises
-
loss of bowel or bladder control
-
clenched teeth
-
irregular breathing
-
unusual behavior
-
difficulty speaking
-
distant or “daydreaming” appearance
Furthermore, status epilepticus may present with nonmotor simple partial seizures characterized by subjective sensory disturbances such as focal paresthesias or numbness, focal visual changes like flashing lights, hallucinations involving taste or smell, and atypical sensations in the abdomen. A form of focal status epilepticus affecting the motor cortex, can manifest as intermittent involuntary twitching of specific muscle groups, often in the face or hand, or as a gradual loss of unilateral function associated with neurological decline.
Complex partial status epilepticus may exhibit recurrent recognizable seizures without recovery between episodes (Type I), or continuous, ongoing seizure activity (Type II). Additional characteristics may include a history of recurrent or prolonged simple partial seizures, confused responsiveness, impaired memory, and clinical automatisms such as repetitive lip-smacking or swallowing movements.
Diagnosis
-
Comprehensive Assessment: Diagnosing status epilepticus entails a thorough evaluation by a healthcare provider, involving a detailed physical examination and a comprehensive review of the patient’s medical history, current medications, and substance usage.
-
Electroencephalogram (EEG): In addition to the initial assessment, an EEG may be conducted, a painless procedure that measures the brain’s electrical activity by placing electrodes on the scalp.
-
Further Diagnostic Tests: Additional tests may be necessary to uncover potential underlying causes. These may include a lumbar puncture (spinal tap) to detect signs of infection, as well as imaging studies such as CT or MRI scans to identify structural abnormalities in the brain.
Blood Tests: Blood tests may also be conducted to evaluate metabolic imbalances, assess immune system function, and detect any toxins or poisons that could contribute to seizures.
Treatment
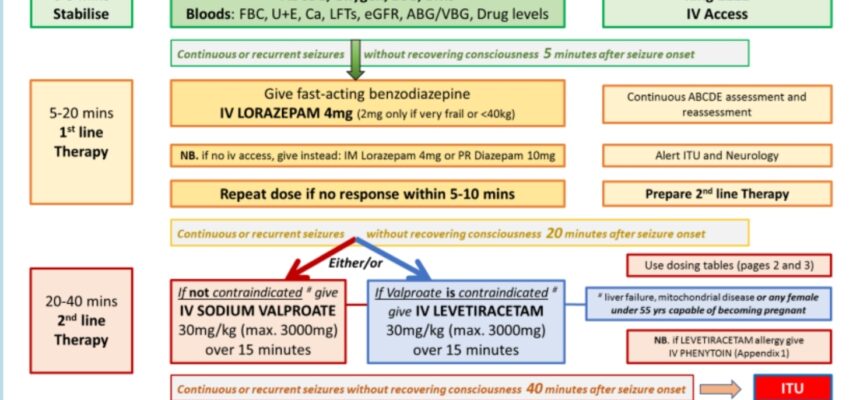
Initial Management:
- Medications:
-
-
Benzodiazepines
-
Antiseizure Drugs
-
-
- Administration of oxygen.
- Blood tests to assess metabolic status.
- Establishment of an intravenous (IV) line.
- Glucose administration if hypoglycemia is suspected as a trigger.
Addressing Provoked Seizures:
● Treating underlying triggers such as medication-related issues, metabolic disturbances, or toxin exposure.
● Antiseizure Treatments:
-
-
Medications: Preventing recurrent seizures and reducing seizure frequency.
-
Surgical Interventions: Epilepsy surgery to manage refractory cases.
-
Dietary Modifications: Implementing ketogenic diets to control seizures.
-
Nervous System Stimulation: Utilizing deep brain or vagus nerve stimulation techniques.
-
Individualized Treatment Plans:
- Tailored approach based on the patient’s specific condition and medical history.
- Recommendations provided by healthcare providers or authorized medical decision-makers.
References
WileyOnline Library: A definition and classification of status epilepticus – Report of the ILAE Task Force on Classification of Status Epilepticus: https://onlinelibrary.wiley.com/doi/full/10.1111/epi.13121
NIH National library of Medicine: Status epilepticus: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2824929/
Cleveland clinic: Status Epilepticus: https://my.clevelandclinic.org/health/diseases/24729-status-epilepticus
Medscapse: Status Epilepticus: https://emedicine.medscape.com/article/1164462-overview
Johns Hopkins Medicine:https://www.hopkinsmedicine.org/health/conditions-and-diseases/status-epilepticus
Cedars Sinai: https://www.cedars-sinai.org/health-library/diseases-and-conditions/s/status-epilpeticus.html
Verified by Dr. Petya Stefanova