Types and Characteristics of Brain Tumors
Normally, cells undergo controlled growth and division, replenishing old or damaged cells in a regulated manner. However, tumor cells exhibit uncontrolled proliferation for reasons not entirely elucidated.
A primary brain tumor is an abnormal mass originating within the brain and typically does not metastasize to distant sites in the body. These tumors can be categorized as either benign or malignant.
Benign brain tumors exhibit slow growth, well-defined margins, and limited capacity for spreading. Despite lacking malignant characteristics, benign tumors may pose a threat to life if they impinge on vital brain structures.
In contrast, malignant brain tumors grow rapidly, possess irregular margins, and have the potential to invade neighboring brain regions. While often referred to as brain cancer, malignant brain tumors do not meet the conventional definition of cancer as they do not metastasize to organs beyond the brain and spinal cord.
Metastatic brain tumors, also known as secondary brain tumors, originate from cancers elsewhere in the body and disseminate to the brain via the bloodstream. These tumors arise when cancer cells are transported through the circulatory system. Common primary sites for metastatic brain tumors include the lungs and breasts.
Central Nervous System (CNS) Tumor Classification:
In contrast to many tumors, CNS tumors are not typically staged using traditional methods like the TNM system due to the unique anatomical characteristics of the brain. The absence of lymphatics in the brain limits tumor spread beyond the CNS, rendering staging less applicable. Consequently, CNS tumor classification heavily relies on accurate grading to assess tumor behavior and prognosis.
Grading and Classification of CNS Tumors
Tumor grade, typically ranging from I to IV, serves as an indicator of the tumor’s aggressiveness. Lower-grade tumors (I-II) are generally less aggressive, while higher-grade tumors (III-IV) tend to exhibit more aggressive behaviour. Pathologists depending on evolution, appearance, growth and malignancy, to assign a specific grade.
Glioma Tumors
About 30% of all central nervous system (CNS) tumors are gliomas, and about 50% of CNS tumors in children are gliomas. A glioma forms as a result of uncontrollable growth in glial cell (the supporting cells of the brain), are the most common type of CNS tumors in children. Can be non cancerous or cancerous. They encompass various subtypes, including:
● Astrocytomas: some can spread widely throughout the brain and blend with the normal brain tissue, which can make them hard to remove by surgery. Sometimes they spread along the cerebrospinal fluid pathways. Can be low grade (I or II), or high grade (III and IV).
● Oligodendrogliomas. Grade II tumors that tend to grow slowly, but most of them can grow into nearby brain tissue and can’t be removed completely by surgery. About 1% of children tumors.
● Ependymomas. About 5% of brain tumors in children. Can range from grade I to grade III tumors. Can spread along CSF pathways but do not spread outside the brain or spinal cord.
Meningiomas
Meningiomas originate in the meninges, the protective layers of tissue enveloping the outer regions of the brain and spinal cord. Accounting for approximately one-third of primary brain and spinal cord tumors, meningiomas represent the most prevalent type of primary brain tumor in adults, although they are not strictly categorised as brain tumors.
These tumors are more commonly diagnosed in older individuals, with the risk increasing with age. Furthermore, meningiomas exhibit a higher incidence in women, occurring approximately twice as often as in men. In some cases, there may be a familial predisposition to developing meningiomas, particularly among individuals with neurofibromatosis, a genetic condition characterized by the formation of multiple benign tumors originating from nerve tissue. Can be classified as Grade I,II, or III based on how the cells look under the microscope.
Diagnostic Features and Characteristics
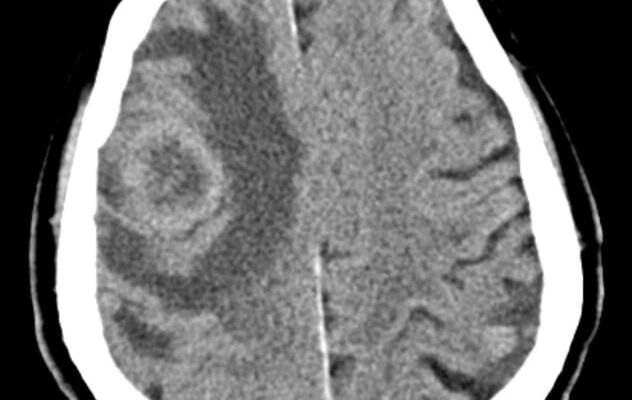
Key diagnostic features of brain tumors include the presence of a tumor core containing actively proliferating malignant cells, necrotic regions, and perifocal edema caused by fluid buildup around the tumor core. These features aid in distinguishing between low-grade gliomas and more aggressive tumors like glioblastoma multiforme (GBM).
Symptoms
Symptoms of a brain tumor can be broadly categorized as general or specific. General symptoms arise due to the tumor’s pressure on the brain or spinal cord, while specific symptoms occur when a particular brain region functions inadequately due to the tumor. Many individuals diagnosed with a brain tumor sought medical attention following issues like headaches or other alterations.
Brain tumors don’t always cause symptoms. In fact, the most common brain tumor in adults, meningioma, often grows so slowly that it goes unnoticed. Tumors may not start causing symptoms until they become large enough to interfere with healthy tissues inside the brain.
General Symptoms of a Brain Tumor
● Headaches, which may be severe and exacerbate with activity or in the early morning.
● Seizures, which may manifest in various forms. Different types of seizures include:
- Myoclonic: Single or multiple muscle twitches, jerks, or spasms
- Tonic-Clonic: Loss of consciousness and body tone followed by twitching and muscle relaxation known as contractions. Additionally, loss of bladder control may occur, along with a brief period of no breathing and changes in skin coloration.
- Sensory: Alterations in sensation, vision, smell, or hearing without losing consciousness
- Complex partial: May lead to loss of awareness or partial or complete loss of consciousness, often associated with repetitive, unintentional movements like twitching.
● Personality or memory changes
● Nausea or vomiting
● Fatigue
● Drowsiness
● Sleep disturbances
● Memory impairment
● Changes in gait or ability to perform daily tasks
Noncancerous brain tumors tend to induce symptoms that develop gradually, often referred to as benign brain tumors. Conversely, cancerous brain tumors provoke symptoms that escalate swiftly, termed brain cancers or malignant brain tumors. These tumors cause symptoms that emerge suddenly and worsen within days or weeks.
Main characteristics of increased intracranial pressure (ICP) in patients with cerebral tumors:
- Headache: Persistent, throbbing headache that is often worse in the morning and may be accompanied by nausea and vomiting.
- Papilledema: Swelling of the optic disc due to elevated ICP, leading to visual disturbances.
- Altered Mental Status: Patients may experience drowsiness, confusion, and, in severe cases, coma as ICP rises.
Early recognition and management are crucial to prevent complications associated with elevated ICP.
Brain Tumor Headaches
Headaches represent the most common symptom of brain tumors. They may arise if a growing tumor presses on healthy cells or causes brain swelling, increasing intracranial pressure. Brain tumor-induced headaches are often worse upon waking in the morning and may intensify with coughing or straining. People with brain tumors frequently describe the headache as resembling tension headaches or migraines. The location of the tumor may also affect the characteristics of the headache. Headache intensity increases within weeks or months.
Specific symptoms depending on the location
● Frontal lobe tumors can induce: alterations in behavior and emotions;
compromised judgment, motivation, or restraint; diminished olfactory perception or
visual impairment; hemiplegia; cognitive decline and memory impairment.
● Parietal lobe tumors may result in: speech impairment; difficulties in writing,
drawing, or naming objects; failure to recognize familiar entities; spatial disorientation
and impaired eye-hand coordination.
● Occipital lobe tumors might precipitate: vision loss in one or both eyes; deficits in
visual field perception; blurred vision, visual distortions, or hallucinations.
● Temporal lobe tumors could lead to: linguistic challenges encompassing difficulty in speech comprehension and expression; memory deficits spanning short-term and
long-term memory; heightened aggression.
● Brainstem tumors may evoke: alterations in behavior and emotions; challenges in
speaking and swallowing; drowsiness; hearing impairment; unilateral facial muscle weakness (e.g., head tilting, crooked smile); unilateral body muscle weakness; unsteady gait; ptosis or diplopia; and nausea and vomiting.
● Pituitary gland tumors might trigger: excessive hormone secretion (e.g., Cushing’s Disease, acromegaly); cessation of menstruation; abnormal milk production; and diminished libido.
Diagnosis
The process of diagnosing a brain tumor typically involves various imaging tests aimed at distinguishing whether the tumor originates within the brain or is a manifestation of cancer that has spread from elsewhere in the body. These tests utilize advanced technology to generate detailed images of the body’s internal structures. Factors such as the suspected type of tumor, the patient’s symptoms, age, overall health, and the outcomes of previous medical assessments are considered when selecting the appropriate diagnostic and treatment approach.
The majority of brain tumors are identified following the onset of symptoms. Often, the initial diagnosis is made by an internist or a neurologist, specialists respectively focusing on adult care and brain and central nervous system disorders. In addition to comprehensive medical history inquiries and physical examinations, the physician may recommend the following tests to ascertain the presence, type, or grade of a brain tumor:
Neurological examination
This comprehensive examination encompasses a battery of tests aimed at elucidating various aspects of nervous system integrity, including motor function, balance, coordination, reflexes, sensation, cranial nerves and cognitive functions.
These meticulous evaluations serve to delineate the neurological status of individuals suspected of harboring a brain tumor, facilitating timely diagnosis and appropriate management strategies.
Computed Tomography (CT) scan
Often CT is the first imaging test performed and where a mass is identified. This imaging technique employs x-rays from various angles to create a detailed 3-dimensional image of the body’s internal structures. It is particularly useful for identifying abnormalities, measuring tumor size, and detecting bleeding or fluid accumulation in the brain. Usually an MRI should be performed to get more detailed pictures.
Magnetic Resonance Imaging (MRI)
MRI is essential in diagnosing a brain tumor. Utilizing magnetic fields rather than x-rays, MRI produces intricate images of the body’s internal structures. A contrast medium, administered intravenously, enhances the clarity of these images. Various MRI techniques, such as diffusion-weighted imaging and perfusion imaging, provide additional insights into the tumor’s cellular composition and blood supply.
Positron Emission Tomography (PET) or PET-CT scan
PET scans utilize radioactive substances to produce images of organs and tissues. They are used to assess tumor activity during treatment and to monitor recurrence.
Cerebral arteriogram
This x-ray procedure visualizes the brain’s arteries after injecting a contrast medium into the bloodstream. It helps assess blood flow to the brain and detect abnormalities. It hels distinguish tumor from aneurysm which sometimes can be considered in the differential diagnosis.
Lumbar puncture or spinal tap
This procedure involves extracting cerebrospinal fluid from the lower back to detect cancer cells or tumor markers indicative of brain tumor spread. It is contraindicated if there is a big tumor mass and increased intracranial pressure because of the risk of brain herniation.
Myelogram
This test involves injecting a contrast dye into the cerebrospinal fluid surrounding the spinal cord to visualize spinal cord abnormalities.
Biopsy
If the findings from imaging scans do not provide a definitive diagnosis, a biopsy may be recommended to ascertain the specific nature of the tumor. Biopsy entails the extraction of a small sample of tumor tissue for microscopic examination by a pathologist. This procedure can be conducted as part of a surgical intervention aimed at tumor removal or as a distinct diagnostic measure, commonly referred to as a needle biopsy.
Additionally, biomarker testing of tumor samples may identify specific genetic or protein alterations unique to the tumor, aiding in prognosis and treatment planning. Neurological, vision, and hearing tests, as well as electroencephalography (EEG) and evoked potentials, assess brain function and detect potential complications associated with the tumor.
Treatment
Surgery
Surgery involves removing the tumor and surrounding healthy tissue. Benefits include symptom relief, providing tissue for diagnosis and analysis, enhancing the effectiveness of other treatments, and improving prognosis.
Indications for brain tumor surgery vary depending on factors like tumor type, size, location, and associated symptoms:
- Resectable Brain Tumors: Surgical removal is recommended for tumors that can be safely excised.
- Tumors Causing Mass Effect or Neurological Deficits: Surgery helps relieve pressure on surrounding brain tissue.
- Intractable Seizures: Surgery may be considered for epilepsy control.
- High-Grade Malignancy: Aggressive tumors often require surgical intervention.
- Hydrocephalus: Tumors causing fluid buildup may necessitate surgery.
- Visual Disturbances: Tumors affecting vision may require removal.
- Hormonal Imbalances: Some tumors affect hormone production.
- Significant Pain: Surgery can alleviate tumor-related pain.
Contraindications for Brain Tumor Surgery:
- Inoperable Tumors: Some tumors cannot be safely removed.
- Poor General Health or High Surgical Risk: Patient factors may preclude surgery.
- Advanced Age: Consider overall health and life expectancy.
- Tumors in Critical or Eloquent Brain Areas: Surgery may cause irreversible deficits.
- Metastatic Brain Tumors with Widespread Disease: Palliative care may be more appropriate.
- Patient Refusal: Respect patient autonomy.
- Severe Comorbidities: Evaluate overall health status.
Overall, the decision for brain tumor surgery involves a multidisciplinary approach, considering tumor characteristics, patient’s health, treatment goals, and risks and benefits of surgery within comprehensive cancer care.
Radiation Therapy
Radiation therapy uses high-energy x-rays or particles to destroy tumor cells, often after surgery and sometimes with chemotherapy or immunotherapy. Techniques include external-beam radiation therapy, 3D conformal radiation therapy, intensity modulated radiation therapy, proton therapy, and stereotactic radiosurgery.
Side effects, like fatigue and skin reactions, are usually temporary. Long-term effects depend on radiation dose and may include memory and hormonal changes.
Medication Therapies
Medications like chemotherapy and targeted therapy destroy tumor cells. They can be given orally, intravenously, or locally. Chemotherapy uses drugs to inhibit tumor growth and can be part of multimodal treatment plans, especially for aggressive tumors.
Chemotherapy drugs vary, with temozolomide being common for brain tumors. Combination therapies like PCV or Gliadel wafers are also used.
Side effects include fatigue, infection risk, nausea, hair loss, and appetite changes. Monitoring with MRI scans helps track treatment effectiveness.
Targeted therapy
Alternative to conventional chemotherapy, targeted therapy focuses on specific genes, proteins, or tissue environments crucial for tumor growth. By pinpointing these targets, this therapy inhibits tumor cell proliferation while minimizing harm to healthy cells.
Each tumor possesses unique targets, and some may harbor multiple ones. Biomarker or molecular testing aids in identifying these factors, facilitating personalized treatment selection. Ongoing research explores novel treatments targeting specific molecular pathways.
References
Scientific report: Classification of brain tumours in MR images using deep spatiospatial models: https://www.nature.com/articles/s41598-022-05572-6
American association of neurological surgeons: Brain Tumors: https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Brain-Tumors
Medscape: Brain Cancer Staging: https://emedicine.medscape.com/article/2006770-overview
Johns Hopkins medicine: Grading and classification:
https://pathology.jhu.edu/brain-tumor/grading-classification
Meyfield brain and spine: Brain tumors: an introduction
https://mayfieldclinic.com/pe-braintumor.htm
American cancer society: Types of Brain and Spinal Cord Tumors in Children
https://www.cancer.org/cancer/types/brain-spinal-cord-tumors-children/about/types-of -brain-and-spinal-tumors.html https://www.cancer.org/cancer/types/brain-spinal-cord-tumors-adults/about/types-of-b rain-tumors.html
University of Colorado cancer center: Brain and spinal cord cancer: https://medschool.cuanschutz.edu/colorado-cancer-center/for-patients-families/cancers-we-treat/brain-and-spinal-cancers
Cancer.Net: Brain Tumor: Symptoms and Signs: https://www.cancer.net/cancer-types/brain-tumor/symptoms-and-signs
Cancer.Net: Brain Tumor: Diagnosis https://www.cancer.net/cancer-types/brain-tumor/diagnosis
Brain Tumor: Types of Treatment https://www.cancer.net/cancer-types/brain-tumor/types-treatment#surgery
Verified by Dr. Petya Stefanova