The internal capsule is a critical white matter structure in the brain, serving as a conduit for numerous motor and sensory fibers traveling to and from the cortex. Damage within this region can lead to distinct clinical findings. Here are the key points:
1. Location of the Internal Capsule:
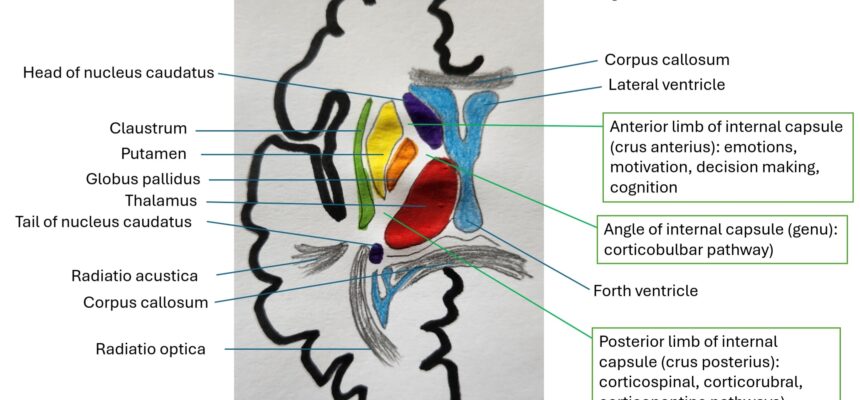
The internal capsule lies within the subcortical structures of the brain.
It consists of three parts:
-
-
- Anterior limb: Separates the caudate nucleus and lenticular nucleus (putamen and pallidum). It contains fibers responsible for the emotions, cognition, motivation and decision making).
- Genu (angle): Contains corticobulbar fibers (from cortex to brainstem).
- Posterior limb: Separates thalamus and lenticular nucleus. Carries corticospinal fibers (from cortex to spine) and sensory fibers (from thalamus to postcentral gyrus).
-
Blood supply to the internal capsule:
-
-
- Anterior limb: Mainly supplied by lenticulostriate branches of the middle cerebral artery (MCA).
- Genu: Also fed by lenticulostriate branches of the MCA.
- Posterior limb: Receives blood from lenticulostriate branches of the MCA and the anterior choroidal artery (AChA) of the internal carotid artery.
-
2. Clinical Findings in Internal Capsular Stroke:
Pure Motor Stroke:
-
-
- Infarction in the internal capsule leads to weakness of the face, arm, and/or leg.
- Upper motor neuron signs include hyperreflexia, Babinski sign, Hoffman sign, clonus, and spasticity.
- This is the most common lacunar syndrome associated with internal capsule infarcts.
-
Mixed Sensorimotor Stroke:
-
-
- Damage to the posterior limb affects both motor and sensory fibers.
- Results in contralateral weakness and contralateral sensory loss.
-
Distinguishing subcortical (internal capsule) from cortical strokes:
- Cortical leg area (supplied by the anterior cerebral artery) vs. cortical arm area (supplied by the middle cerebral artery).
- Cortical strokes produce additional symptoms not commonly seen in subcortical lesions.
-
Thalamic Syndrome
The thalamus is a small, paired structure located deep within the brain, situated between hypothalamus, midbrain, epithalamus (including the pineal gland), internal capsule, and basal ganglia. It consists of > 50 gray matter nuclei.
Thalamic nuclei play diverse functional roles:
-
- Reticular and intralaminar nuclei: Involved in arousal and nociception.
- Sensory nuclei: Process sensory information.
- Effector nuclei: Control motor function and aspects of language.
- Associative nuclei: Participate in high-level cognitive functions.
- Limbic nuclei: Influence emotions and memory.
Blood supply
The blood supply of the thalamus primarily comes from branches of the posterior cerebral artery (PCA), which is a major branch of the basilar artery.
Thalamic syndromes
A thalamic syndrome refers to a constellation of neurological symptoms caused by damage or dysfunction in the thalamus, a central structure within the brain. Thalamic syndromes can result from various conditions, including stroke, trauma, tumors, infections, or degenerative diseases affecting the thalamus.
Common features of thalamic syndromes include:
1. Sensory Disturbances: Thalamic syndromes often manifest with sensory abnormalities, such as sensory loss or altered sensation, typically on the contralateral side of the body due to the thalamus’s role in relaying sensory information.
2. Pain: Thalamic pain syndrome, also known as Dejerine-Roussy syndrome, is characterized by severe, persistent, and often unexplained pain on the contralateral side of the body. This pain can be spontaneous, burning, or lancinating in nature.
3. Motor Deficits: Depending on the location and extent of thalamic damage, motor deficits such as weakness or paralysis may occur, although these are less common compared to sensory abnormalities.
4. Cognitive and Behavioral Changes: Thalamic syndromes can also lead to cognitive impairments, including memory deficits, executive dysfunction, and changes in mood or behavior. These changes can vary depending on the specific thalamic nuclei affected.
5. Eye Movement Abnormalities: Lesions involving certain thalamic nuclei may result in eye movement abnormalities, such as nystagmus or gaze palsies.
6. Hemiballismus: Damage to the subthalamic nucleus, which is closely associated with the thalamus, can cause involuntary flinging movements of one side of the body known as hemiballismus.
Thalamic syndromes can vary widely depending on the location and extent of thalamic damage, as well as individual differences in neuroplasticity and compensatory mechanisms.
References:
(1)stanfordmedicine25.stanford.edu
(2)radiopaedia.org
(3)ahajournals.org
(4)verywellhealth.com
Verified by Dr. Petya Stefanova