Alexander Z
Student
Fragen
Resümees
Videos
Audios
In which lighting condition is pupillary inequality due to Horner’s syndrome most obvious?
Oktober 11, 2024
When should myasthenia gravis be considered in a patient with weakness of eye movements?
Oktober 11, 2024
In a patient with unilateral Horner’s syndrome present from birth, what is a possible characteristic of the affected eye?
Oktober 11, 2024
Ptosis associated with weakness of orbicularis oculi is most likely due to which of the following conditions?
September 28, 2024
Which of the following conditions is least likely to cause complete ptosis, where the pupil is covered by the lid?
September 5, 2024
What is the essential feature of a positive Romberg’s sign?
August 26, 2024
In acute facial weakness, which muscle may be weak for a few days, making it indistinguishable from a lower motor neuron (LMN) weakness?
August 26, 2024
Which of the following symptoms is uncommon in facial nerve lesions?
August 26, 2024
Which of the following statements is true regarding facial nerve palsy after temporal bone fractures?
August 26, 2024
In multiple sclerosis (MS), which type of facial palsy is commonly observed, unlike weakness in other muscle groups?
Which of the following statements is true regarding sensation alterations in Bell’s palsy?
August 26, 2024
In Bell’s palsy, why does the affected eye sometimes brim with tears?
August 26, 2024
Which condition should be suspected when a patient presents with bilateral facial weakness, unblinking expression, and a “horizontal” smile (inability to elevate the angles of the mouth)?
August 26, 2024
What is the purpose of Bell’s phenomenon in assessing facial weakness?
August 26, 2024
In the context of Bell’s palsy, which condition should be considered when a child presents with acute facial weakness and a recognized association with hypertension?
What is an essential consideration when evaluating facial palsy?
August 26, 2024
What is the characteristic feature of pes cavus?
August 24, 2024
When assessing eversion and inversion of the foot, what technique should be used to prevent hip rotation?
August 24, 2024
In a patient with absent ankle jerks, what is an important test to perform due to the possibility of cauda equina lesions?
August 24, 2024
What technique can be used to enhance the ankle jerk reflex if it is not readily elicited by tapping the Achilles tendon?
August 24, 2024
Q 2.21. Cerebral Vein and Dural Sinus Thrombosis
Mai 19, 2024
Q 1.28. Peripheral Nervous System (PNS) Syndromes of Damage
Mai 19, 2024
Q 1.18. Syndromes of Parietal Lobe Damage
Mai 18, 2024

Q 1.15. Higher Cortical Functions. Gnosis and Agnosia. Praxis and Apraxia.
Mai 13, 2024
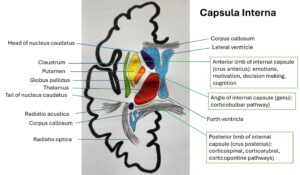
Q 1.21. Internal Capsule Syndromes. Thalamic syndrome.
Mai 13, 2024

Q 1.27. Autonomic nervous system: anatomy and physiology. Impairment syndromes. Examination methods. Orthostatic intolerance. Horner syndrome.
Mai 2, 2024
Q 1.17. Syndromes of Frontal Lobe Damage
April 24, 2024
Q 1.19. Temporal Lobe Syndromes
April 24, 2024
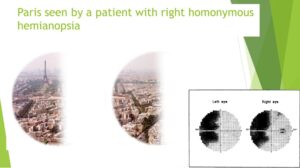
Q 1.20 Syndromes of Occipital Lobe Damage
April 24, 2024
Q 1.23. Brainstem Syndromes: Pons
April 24, 2024

Q 1.24. Brainstem Syndromes: Mesencephalon
April 23, 2024
Q 1.25. Spinal Cord: Anatomy, Physiology, and Blood Supply
April 7, 2024
Q 1.22. Brainstem Vascular Syndromes: Medulla Oblongata
April 7, 2024
Q 1.29. Syndrome of meningeal irritation. Examination methods. Syndrome of increased intracranial pressure.
April 7, 2024
Q 1.31. Anatomy and Physiology of Cerebrospinal Fluid (CSF). CSF Syndromes.
März 31, 2024
Q 2.6. Polyneuritis and Polyneuropathies. Toxic and Deficiency Neuropathies.
März 31, 2024
No videos found
Question 1: Peripheral Nervous System Disorders. Classification. Neuralgia, mononeuritis, plexitis. Treatment.
Radiographic Evaluation of the Cranium
Februar 2, 2024