Mesencephalon (Midbrain):
-
- The mesencephalon is the smallest part of the brainstem, located cranially.
- Embryologically, it develops from the neural ectoderm and forms a critical connection between the cerebrum, cerebellum, and spinal cord.
Here’s an overview of midbrain structures and the symptoms observed with lesions in these areas:
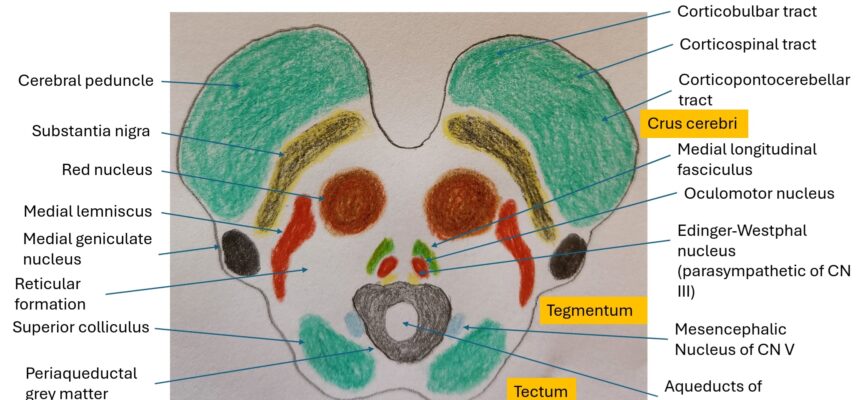
1. Tectum:
– Comprises the superior and inferior colliculi.
– Lesions can lead to visual and auditory deficits.
– Damage to the superior colliculus can cause impaired visual reflexes, such as difficulty tracking moving objects or saccadic eye movements.
– Damage to the inferior colliculus can result in auditory processing deficits, affecting the ability to localize sound sources.
2. Tegmentum:
– Includes nuclei and fiber tracts involved in motor and sensory functions, as well as arousal and consciousness.
– Lesions in this area can lead to various motor and sensory deficits, depending on the structures affected.
– Damage to the red nucleus can result in contralateral tremors and movement disorders.
– Lesions affecting the substantia nigra can lead to Parkinsonian symptoms.
– Damage to the medial longitudinal fasciculus (MLF) can cause internuclear ophthalmoplegia (INO), characterized by impaired adduction of the ipsilateral eye on horizontal gaze.
3. Cerebral Peduncles:
– Contain descending motor fibers such as the corticospinal and corticobulbar tracts.
– Lesions can lead to contralateral motor deficits.
– Damage to the corticospinal tract can result in contralateral hemiparesis or hemiplegia, as seen in Weber syndrome.
4. Crus Cerebri:
– Houses motor and sensory fibers traveling to and from the cerebrum.
– Lesions can lead to various motor and sensory deficits, depending on the structures affected.
– Damage to the oculomotor nerve (CN III) can result in ipsilateral ptosis, diplopia, and impaired extraocular movements, as seen in Weber, Benedict, and Claude syndromes.
– Compression of the oculomotor nerve can also cause dilation of the pupil (mydriasis) and loss of pupillary light reflex.
Some of the wellknown mesencephalon syndromes are:
Weber Syndrome:
- Characterized by:
– Ipsilateral oculomotor nerve (CN III) palsy.
– Contralateral hemiparesis or hemiplegia due to involvement of the cerebral peduncle.
- Often caused by:
– Occlusion of the posterior cerebral artery.
Internuclear Ophthalmoplegia (INO):
- Characterized by:
– Impaired adduction of the ipsilateral eye on attempted horizontal gaze.
– Convergence usually unaffected.
- Typically caused by:
– Lesions affecting the medial longitudinal fasciculus (MLF), often due to multiple sclerosis.
Benedict Syndrome:
- Characterized by:
– Ipsilateral oculomotor nerve (CN III) palsy.
– Contralateral cerebellar ataxia.
- Resulting from:
– Lesions affecting the midbrain tegmentum, often due to vascular events or tumors.
Claude Syndrome:
- Characterized by:
– Ipsilateral oculomotor nerve (CN III) palsy.
– Contralateral ataxia and tremor.
- Usually resulting from:
– Lesions affecting the tegmentum of the midbrain, commonly due to vascular pathology.
Parinaud Syndrome:
- Characterized by:
– Vertical gaze palsy, often with an upward gaze palsy.
– Convergence-retraction nystagmus.
– Light-near dissociation of pupils.
- Typically due to:
– Compression or damage to the dorsal midbrain, often by tumors or pineal gland masses.
________________________
Remember the Rule of 4:
-
-
- 4 structures in the midbrain (CN III, IV, V, VI).
- 4 structures in the pons (CN V, VI, VII, VIII).
- 4 structures in the medulla (CN IX, X, XI, XII).
-
This simplified approach helps localize the affected artery and understand the distinguishing features of each syndrome.
-
References:
(1)ncbi.nlm.nih.gov
(2)researchgate.net
(3)radiopaedia.org
Verifiziert von Dr. Petya Stefanova